“Staff Nurses Change Practice”
Evidence Based Practice is a way of thinking. Being a professional autonomous nurse means purposefully providing the best care possible for each and every patient. Evidence Based Practice (EBP) combines three tenets. The first is using the best available scientific evidence; the second is clinician expertise; the third, patient preference (Levin & Feldman, 2006). Most nurses strive to provide the best care possible for the patients served; integrating EBP into practice improves nursing care. A framework for guidance to discover and implement best practice assists nurses to meaningfully integrate the three tenets of EBP into everyday patient care.
I am lucky that in the institution in which I work, the shared governance model provides the framework to discover and implement best practice. I have shared in previous articles in Up to Par about my work on undiagnosed obstructive sleep apnea in the adult perioperative population. I was led to investigate the issue because of problems with breathing and hypoxia in some of our post anesthesia patients. The Evidence Based Practice and Nursing Research Council, particularly the mentor, supports me in my work to improve the care of this patient population.
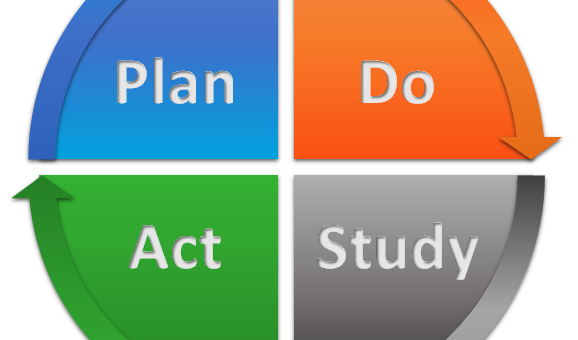
The model used to guide the work of the council and therefore my work, is the Evidence Based Performance Improvement Model (EBPI) by the Visiting Nurse Service of New York and Dr. Rona Levin (see illustration). No matter the issue or problem, the EBPI model can be utilized. So, for example, nurses noted that a number of overweight patients, mostly men with a history of snoring were experiencing airway obstruction and hypoxia in the postanesthesia care unit (PACU) This group of patients was not diagnosed with obstructive sleep apnea (OSA).
I remember hearing about the STOP-Bang tool at an ASPAN national conference. I performed a literature search to find out more about OSA and the STOP-Bang tool. This illustrates the process described in the first three boxes of the EBPI Model. The problem is: some overweight male adult patients experience postoperative airway obstruction and hypoxia. The focused clinical question is: What can be done to prevent or mitigate airway obstruction and hypoxia in this patient population and how can we identify which patients will experience postoperative airway obstruction and hypoxemia? The search for evidence revealed that the STOP-Bang tool provides a reliable method to identify patients at risk for OSA.
The arrows between the “formulate focused clinical question” and the “search for evidence” boxes demonstrate the iterative nature of the process. As new evidence is found, the clinical question may change and as the clinical question changes, new evidence must be sought.
Using a framework such as the EBPI Model can guide staff nurses to change practice to improve patient care and ultimately enhance patient outcomes. I challenge all to give the model a try! In future issues of Up to Par I will discuss the other aspects of the EBPI Model.
Reference Levin, R. F. & Feldman, H. R. (2006). Teaching evidence based practice in nursing. New York, NY: Springer.